Gastroesophageal Reflux Disease
Gastroesophageal Reflux Disease (GERD)
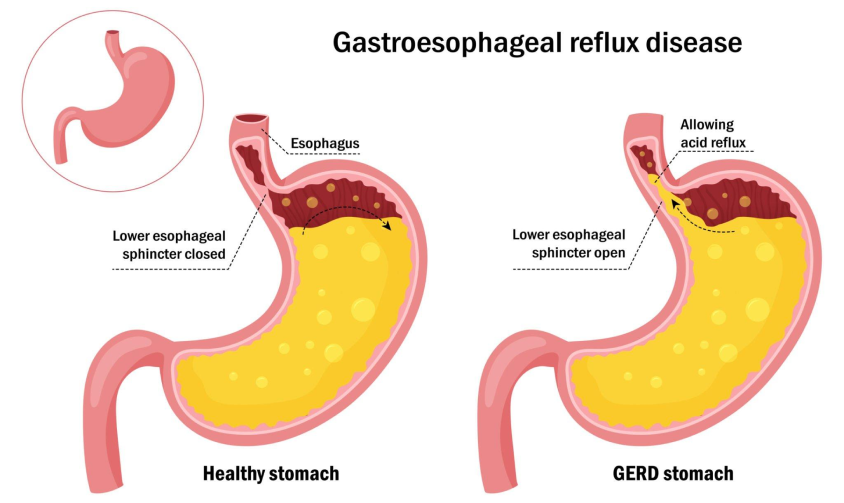
Gastroesophageal Reflux Disease (GERD) is a condition in which the strongly acidic stomach contents are able to flow, or reflux, back up into the esophagus.
The most common symptom of GERD is heartburn, which can significantly impact a person’s quality of life. If left untreated, this can lead to more significant problems such as erosive esophagitis, esophageal strictures, tooth decay, hoarseness of voice, aspiration, and even esophageal cancers.
Treatment of GERD
GERD is generally treated in a stepwise fashion from less invasive strategies to more invasive strategies.
Initial GERD management focuses on optimizing lifestyle factors contributing to GERD such as avoiding caffeine, nicotine products, alcohol, spicy foods, etc. It also involves avoiding eating late at night and sleeping with the head of your bed elevated to allow gravity to help keep stomach contents down.
The next step is addition of medications which included classes of drugs such as proton pump inhibitors, H2 blockers and antacids.
If medications and lifestyle optimization fail to control GERD, or patients are unable to tolerate the medications, or they do not want to be on medications life long, anti-reflux surgery should be considered.
Surgical Treatment for GERD
As the underlying cause of GERD is weakening of the muscular valve between the stomach and esophagus (lower esophageal sphincter) that functions to keep stomach acid down, the primary goal of surgery is to reinforce the valve to prevent acid from refluxing into the esophagus.
This is accomplished through a laparoscopic procedure called a fundoplication, in which the top of the stomach, or fundus, is wrapped around the bottom of the esophagus. If patients have an associated hiatus hernia, where the stomach has herniated through the diaphragm, this will be repaired at the same time. Anti-reflux surgery is highly effective, and over 95% of people are off acid suppressing medications immediately after surgery.
Recovery After Anti-Reflux Surgery
As the surgery is done through 5 mm incisions, patients can expect faster recoveries and significantly less post operative discomfort as compared to traditional open anti-reflux surgery.
Recovery generally entails a single overnight stay in the surgical facility, followed by discharge the following morning. Patients will be required to be on a soft/pureed diet for four weeks after surgery while recovering, at which time, they will be able to return to a fully regular diet.